*** Please note Dr. Rebecca Glaser (USA) is giving a webinar for the European Menopause and Andropause Society 16 October 3:00 PM (Amsterdam EST) on ‘Testosterone – Anastrozole therapy in advanced breast cancer: A case series’.
You can watch it live or register for a replay video here.
____________________________________
For immediate release 29th September 2021
Many people have long suspected there was a simple common-sense therapy for cancer. Testosterone implant therapy has been shown to offer protective properties against breast cancer and safely relieve menopausal symptoms in breast cancer survivors.
Testosterone (in combination with an aromatase inhibitor to prevent the conversion of testosterone to oestrogen) has been used to reduce the size of invasive breast cancers, helping to either avoid the need for invasive breast cancer surgery or lessen the impact of the procedure.
Dr Rebecca L Glaser, MD, FACS, is a retired breast cancer surgeon, who is currently involved in research on testosterone therapy by pellet implant and its impact on health and breast cancer prevention. “This isn’t magic or a complex ‘new molecule’ worth billions of dollars to investors,” she says, “it’s basic science.”
“Estrogen stimulates breast cancer growth – testosterone inhibits breast cancer growth – anastrozole blocks the conversion of testosterone to estradiol – and sugar feeds tumors.”
Not surprisingly, major pharmaceutical companies have shown no interest in the therapy.
“Women come to me for treatment at all different stages of breast cancer. I’ve used testosterone pellets (combined with an aromatase inhibitor) prior to surgery, to help reduce the size of the cancer, so it’s smaller to remove,” she says. “You then have evidence that the tumor responds favourably to testosterone implant therapy, so if the patient chooses, we continue the therapy after surgery, not just for tumor control, but menopausal symptom control as well.”
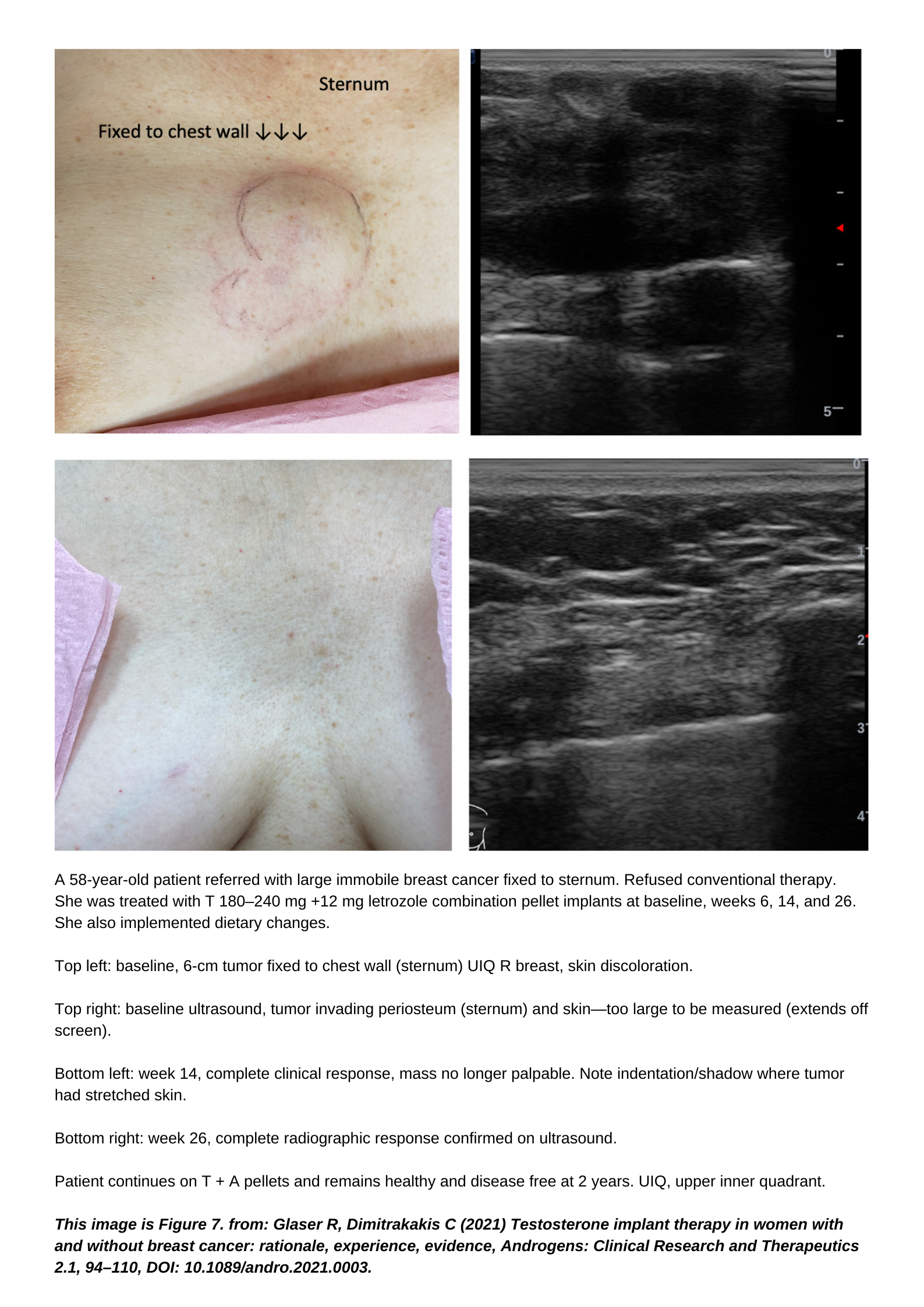
We have also seen breast cancers completely respond to this therapy:
“Patients travel from across the United States to access this treatment – because it works,” says Dr Glaser. “It’s upsetting when a patient with metastatic breast cancer, crippled with bone pain, has to fly from California to Ohio to receive this therapy.”
So why isn’t this treatment readily available for women with breast cancer?
“Number one, doctors just don’t know about it,” says Dr Glaser. “And because it’s not a drug company commercial therapy it’s hard to get information out there. Large clinical trials are extremely expensive and unless there’s a huge profit margin at stake, investors are unlikely to fund trials and market the product.” She believes the only way we can tackle this is from a grass-roots level.
There is also evidence that testosterone protects the nervous system and may benefit patients who have Parkinson’s and Alzheimer’s disease. The first patient Dr Glaser treated with testosterone pellet implants was an elderly man who had Parkinson’s disease. The results were amazing and after a few days he was a different person – his mood, tremors, jaw movements, and walking dramatically improved.
“It’s the method of delivery – unlike topical creams and patches, subcutaneous pellets deliver clinically effective amounts of testosterone to the androgen receptor 24 hours a day, 7 days a week.”
Through her career Dr Glaser has evaluated and treated more than 1500 breast cancer patients and her research publications have been extensively cited (over 2000 citations) including original data on sentinel lymph node biopsy, which is now the standard of care in breast cancer surgery. Her most recent paper, ‘Testosterone Implant Therapy in Women With and Without Breast Cancer: Rationale, Experience, Evidence’ which she co-authored with Dr Constantine Dimitrakakis was published in June 2021.
Testosterone therapy can begin at any stage of breast cancer, Dr Glaser has treated patients who have refused surgery, with testosterone along with an aromatase inhibitor (oestrogen blocker, e.g., anastrozole) combined in the pellet implant if their tumour is oestrogen receptor positive. She’s treated patients with metastatic disease (when the cancer spreads) that she’s been following for years, using testosterone to keep them alive and healthy.
What can be done to make this a therapy that’s accessible for women across the world? Dr Glaser believes that we need to create awareness on the treatment, so women start going to their doctors and asking to try subcutaneous testosterone therapy.
Some consider it ‘alternative’ medicine, but Dr Glaser considers it ‘evidence-based medicine’. “There are many myths and misconceptions about testosterone therapy in women despite the evidence,” she says.
The recent ‘Global Consensus Position Statement on the Use of Testosterone Therapy for Women’ which was published in 2019, currently directs the diagnostic and treatment decisions that our doctors make across the world with regard to the so-called ‘male’ hormone.
Dr Glaser believes the position statement is a cause for concern due to the impact that commercial conflicts of interest might have on these guidelines. The majority of the authors have significant conflicts and ties to the pharmaceutical industry, which also sponsors/funds the societies that published the statement. Plus, she says it also violates many policies that ensure the integrity of such guidelines.
Most concerning, the guidelines fail to acknowledge the preference of many thousands of women who currently benefit from testosterone therapies for breast cancer, menopause symptoms or other age-related diseases.
It has serious ramifications for those women who could be adversely affected if specialists are forced to follow the recommendations and alter their prescribing practices.
“Why aren’t we shouting about this treatment from the rooftops?” asks Susanne Mitchell, author of ‘The Naked Truth About PERIMENOPAUSE’, which takes a deep dive into testosterone therapy as a treatment option for menopausal symptoms. “It’s outrageous that it’s so difficult for women to access this hormone through menopause, and that its success in treating breast cancer and other ageing diseases just isn’t being reported.”
As part of her investigation into testosterone therapy for the book, Mitchell interviewed Dr Glaser, to ask why. She first started to investigate testosterone as a mid-life woman struggling with significant cognitive function and chronic fatigue issues through perimenopause (the 2-10 years prior to menopause). She learned that testosterone and other related hormones in the body – also known as androgens – have important roles in healthy women.
But there’s a common misperception that women’s bodies do not produce much testosterone. Yet it is the most abundant biologically active hormone throughout a woman’s lifespan. Through our lifetime (excluding pregnancy), women make 10 – 15 times more testosterone than oestrogen.
“My cognitive function and fatigue were significantly improved just one week into using topical testosterone cream,” she says. “I contacted Dr Glaser while writing my book and she guided my understanding of the treatment, sent many academic research papers and cast her medical eye over my manuscript.”
Mitchell has since started using the subcutaneous pellets and finds the delivery method works far better than the cream. The author is based in Australia where accessing the pellet implants is extremely difficult. Few doctors are aware of the therapy and the current guidelines actively discourage the use of testosterone in women for anything other than sexual dysfunction.
“It’s something we must address and build awareness around,” says Mitchell. “We need to be talking about this very loudly – demanding to be heard.”
Dr Glaser also introduced the author to Dr Angela DeRosa, DO, MBA, CPE, who shared her broad knowledge with Mitchell, gained from 25 years of clinical practice in women’s hormonal health.

“These are two women doing big things in addressing ‘conventional medical thinking’ promoted by the current guidelines and are working hard to change it,” she says.
“Women face very real gender bias in treatment of their hormonal health and the current guidelines serve to underline the importance of addressing where our information comes from and what might influence that. It’s why I wrote the book, to try and reach as many women as possible,” she says. “If we are more informed, we can make better choices for our health and wellbeing.”
Working from her clinic in Dayton, Ohio, Dr Glaser is a well-respected breast cancer surgeon in the area, where she says her work with testosterone as a therapy for breast cancer patients isn’t always approved of, despite the evidence she continues to present.
“This is considered alternative and controversial, but my patients show enough evidence that many local doctors who didn’t approve in the past have stopped interfering,” says Dr Glaser. “In fact, I have received referrals from some oncologists whose patients could not tolerate oral aromatase inhibitor therapy.”
Testosterone has been used for over eighty years to treat breast cancer and symptoms of hormone deficiency in pre and postmenopausal. Evidence supports that androgens are breast protective.
So where does that leave women who want to explore the possibilities of testosterone therapy? Australia has recently become the first country in the world to approve a female specific testosterone product, a topical cream called AndroFeme® 1. But it is only approved for treating hypoactive sexual desire disorder (HSDD) and not for use in treating symptoms of menopause or breast cancer. Plus, it’s a cream and not a subcutaneous pellet, which is the delivery method Dr Glaser and Dr DeRosa both use in their work in the USA.
“The clinical outcomes were what sold me on pellets,” says Dr Glaser. “I get testimonials from people who say this is great, but when you see people with a serious disease, the pellets can be game changing. It’s the method of delivery, and nothing else does that, not the creams or the patches but the pellets. They mimic the body, delivering adequate amounts of androgens (testosterone) 24 hours a day, 7 days a week.”
One of Dr Glaser’s biggest arguments is that you need to treat the patient and not micromanage the levels in the blood. Testosterone’s effect is ‘dose dependent’, meaning that the higher the dose, the greater the clinical effect. You can’t keep those levels in a normative blood range.
She explains why it makes no sense to keep serum levels in the normative range. “80 per-cent of a female’s bioavailable testosterone comes from the pro-androgens, DHEA(S) and androstenedione, which also decline with age – the amount of testosterone released from the pellet replaces the significant contribution from all of the androgens, not just testosterone.”
“Enough testosterone needs to be available at the androgen receptor (in the target organs) to produce the clinical results. The only way you can tell that is by talking to your patient and asking; how are you feeling? Did your symptoms come back? When? Any side effects?” The dose is adjusted based on the patient’s response to therapy.
So it all comes down to the delivery, to treat ageing diseases, menopause and breast cancer, the pellets give continuous, constant, slow-release delivery of the testosterone.
Pellets are produced by compounding pharmacies under strict regulations, but drug companies continue to fight compounded pharmaceuticals and in the USA the FDA doesn’t approve the use of testosterone in women at all.
Could it be that pharmaceutical companies are protecting their bottom line and using the ‘Global Consensus Position Statement on the Use of Testosterone Therapy for Women’ as a shield? Why? Because you can’t patent-protect a hormone such as testosterone unless you change the chemical structure.
This is why we have so many synthetic (slightly altered chemistry) HRT drugs for example, rather than bioidentical (replicating the exact chemistry our bodies produce). To patent a commercial hormone product, they must change the chemical structure (risking side effects) or offer a unique delivery method of the original molecule.
And if testosterone were more easily accessible, then many prescription drugs that address menopause, breast cancer and ageing diseases would lose sales and profits.

“There appears to be a well-orchestrated attempt by the pharmaceutical industry to eliminate bioidentical hormones as well as the compounding pharmacies that fill the long-standing hormone gender gap which causes women to needlessly suffer,” says Dr DeRosa.
“A billion-dollar industry has been built on dozens of testosterone replacement therapies to treat andropause and erectile dysfunction for men,” she says. “Women have not been as fortunate despite suffering symptoms from a decline in testosterone levels, and the evidence Dr Glaser continues to present in terms of treating breast cancer. It’s outrageous.”
Dr Glaser believes the ‘Global Consensus Position Statement on the Use of Testosterone Therapy for Women’ violates many policies ensuring the integrity of guidelines, including its failure to acknowledge legitimate controversy surrounding the topic. Plus, the data presented included selected industry-sponsored randomised controlled trials (RCTs) but excluded other research such as observational studies.
After reviewing selected RCT’s, and excluding certain data from observational studies, the authors of the statement advised against compounded therapies, dosing, subcutaneous testosterone implants, and injections although no supporting data or ‘evidence of harm’ was presented.
But Dr Glaser says that because it’s not a drug company commercial therapy it’s hard to get it out there. RCT’s are extremely expensive to run, and unless there’s a product that can be patented as an end goal, Big Pharma won’t fund trials. She believes the only way we can tackle this is from a grass-roots level, by women sharing the information and asking their doctors to try the therapy.
By sharing this article with your friends and women in your life, you can help to spread the word.
Patients support this therapy.
“I was diagnosed with breast cancer aged 66, I did not want surgery or chemotherapy,” says one of her patients in a video testimonial. “I saw Dr Glaser and she started me on hormone therapy. I noticed in the first week that there was a decrease in the size of the tumour in my breast. After two years I’ve had significant results. I feel good, I have energy and I have good memory. I’ve not had any surgery, any chemotherapy or radiation.”
Dr Glaser treats a patient with testosterone pellets for under $300 USD, which covers around three months of therapy – chemotherapy costs around $230,000.
“It needs someone with very deep pockets to take an interest and fund an RCT to help make it an established therapy in the treatment of breast cancer,” she says. “All I can do is keep treating my patients, producing more evidence to support the therapy.”
/End
To request an interview with Dr Rebecca Glaser, Dr Angela DeRosa or Susanne Mitchell please call (AEST) +61 403 395 300 or via email here.
A selection of publications and presentations by Dr Rebecca Glaser can be found at http://hormonebalance.org/publications and a full list of her credentials are listed on her CV here.
Download Dr DeRosa’s Media Kit here.
Review copies of ‘The Naked Truth About PERIMENOPAUSE’ are available on request
The book is available as a print and e-book through all major book retailers including: Booktopia, Barnes & Noble, Waterstones and Amazon
The e-book is also available direct from the author:
www.susanne-mitchell.com/bookshop

